INTRODUCTION
Pathology is the study and diagnosis of disease via the examination of body tissue, which is typically fixed on glass slides and viewed under a microscope
Digital Pathology describes the creation, viewing, management, sharing, analysis, and interpretation of virtual images of glass slides and includes workflow considerations specific to a digital imaging environment.
The use of computer-based technology, digital pathology utilizes virtual microscopy.
Glass slides are converted into digital slides that can be viewed, managed, shared and analyzed on a computer monitor.
With the practice of Whole-Slide Imaging (WSI), which is another name for virtual microscopy,The area of digital pathology is developing and has pakages in diagnostic medicine, with the goal of achieving efficient and cheaper diagnoses, prognosis, and prediction of diseases
WSI devices have become essential tools that could aid habitual diagnostic work and scientific discovery in pathology and have enabled the development of next‑generation tools including artificial intelligence (AI)
Photo credit: https://www.medgadget.com/2018/09/digital-pathology-market-overview-by-top-leaders-exclusive-data-of-industry-size-recent-trends-and-growth-analysis-up-to-2023.html
EVOLUTION OF MICROSCOPE
700BC - Nimrud lens
1020 - Books of optics
1590 - Early microscope
1609 - Compound microscope
1625 - First term "microscope"
1665 - First term "cells"
1932 - Phase contrast microscope
1986 - Nobel prize for microscope
2014 - Chemistry, Nobel prize for super microscope
USES CASES
LIMITATIONS OF COMPOUND MICROSCOPE
Optical microscopes are the oldest layout of microscope and were possibly invented in their present compound shape in the 17th century.
Basic optical microscopes can be very simple, although many complex designs aim to improve resolution and sample contrast.
At very high magnifications with transmitted light, point objects are seen as fuzzy discs surrounded by diffraction rings.
Surpassing the resolution limit
Multiple techniques are available for achieving resolutions higher than the transmitted light limit.
Holographic techniques, as defined by Courjon and Bulabois in 1979, are also capable of breaking this resolution limit, although resolution was restricted in their experimental analysis.
While most techniques focus on increases in lateral resolution there are also some techniques which aim to allow analysis of extremely thin A routine (non-digital) pathology workflow usually
VIRTUAL MICROSCOPY
Virtual microscopy is a technique of posting microscope images on, and transmitting them over, computer networks.
This permits unbiased viewing of images by massive numbers of people in diverse locations. It involves a synthesis of microscopy technologies and digital technologies.
The use of virtual microscopes can transform traditional teaching methods by removing the reliance on physical space, equipment, and specimens to a model that is solely dependent upon computer-internet access.
This increases the convenience of accessing the slide sets and making the slides available to a broader audience.
Digitized slides can have a high resolution and are resistant to being damaged or broken over time.
TRADITIONAL PATHOLOGY
A routine (non-digital) pathology workflow usually involves the procurement of tissue, processing of tissue and creating or developing of glass slides.
The pathologist is tasked with the interpretation of glass slides locally inside each hospital or a pathology group which may be serving several hospitals.
This workflow is manual and calls for many steps. The end result is that these glass slides are moved around and sent to pathologists to render a diagnosis.
This may be a time consuming and high prized system as slides are moved around, particularly if the pathologist is not directly in the local area where the slides are prepared.
In some instances, unique cases are sent from the general/community pathologist to a sub-specialist/academic pathologist for an over-read consult.
The role of the general pathologist is to render diagnosis at community hospitals.
For cases which are challenging and difficult, these may be sent to an expert for a traditional consult, which may also take days to weeks.
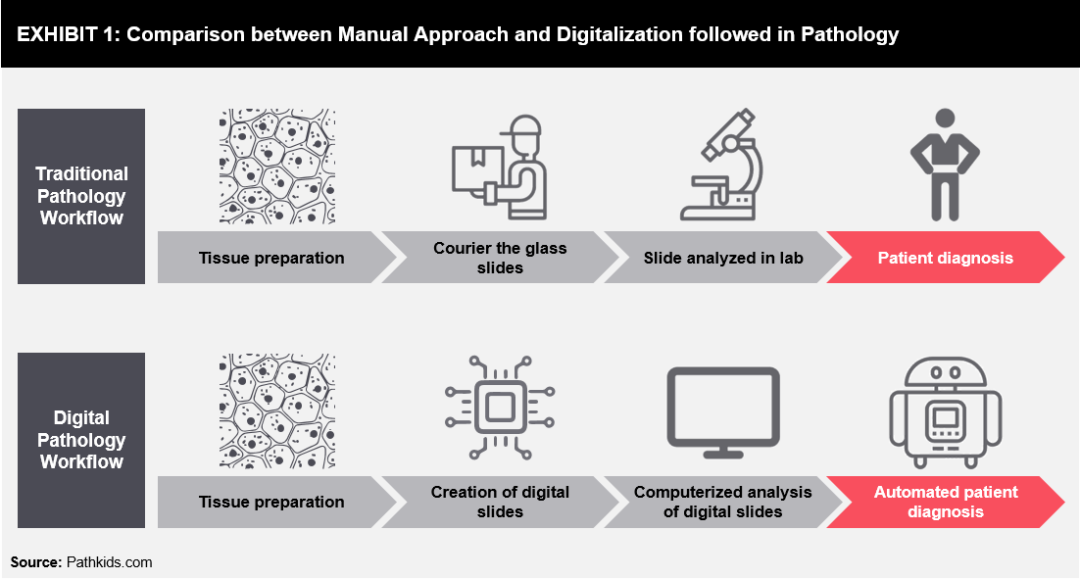
Photo credit: www.pathkids.com
DIGITAL PATHOLOGY
A whole slide imaging scanner can be considered a digital microscope which is outfitted with special high resolution cameras which mixed with optics and software program serve to provide diagnostic quality images.
These images are an accurate representation of the scanned glass slide and in some applications, they may be greater valuable than the real glass slides in terms of image resolution and ease of identification of specific diagnostic features.
Once the slides are digitized and transformed to pixels, the end result is creation of a pixel pipeline which allows pathologists to remotely view the images and share them for a digital consultation.
Overall, it becomes much easier to share these consultation images for diagnostics as well as workflow applications.
The most critical use of these digitized images is to create diagnostic algorithms or applications which can increases the diagnostic workflow.
These images are called whole slide images, digital, or virtual/digital slides. The scanner, typically, uses a proprietary method to capture several resolutions of the complete slide, compress, and save them in an image report designed to rapidly reconstruct the digital slides at different resolutions.
The capture resolution in the scanner determines the maximum effective magnification of the digital slide on a computer monitor.
Most scanners support capture resolutions of 0.5 microns/pixel (powerful viewing magnification: 20X) or 0.275 microns per pixel (powerful viewing magnification: 40X).
The photo file associated with a 20X scan of a 15mmx20mm tissue specimen is as massive as 3.6GB and a 40X scanned image can be as large as 14.5GB.
The images are compressed to more manageable sizes (25:1 compression or greater) such that there is an optimization between image quality, image file length , network bandwidth usage, and server and client resource utilization. For example, the 20X scan could be stored in a JPEG2000-compression file of size 144MB.
The 40X image described above could be stored in a JPEG2000-compressed file of size 576MB. Digital Pathology images are about 10X that of Radiology images and will require more storage management through their useful life cycle.
In order to facilitate the digital workflow, the DPS additionally stores, retrieves, displays, and manages metadata associated with digital slides.
At the scanner, metadata such as the macro image, scan parameters, scan plan, and tissue map are generated and related to the image.
When the DPS is incoprated with an AP-LIS, then patient, case, and histology (part/block/stain) data can also be retrieved from the LIS. A digital case can be created in the DPS by associating digital slides with the case and histology information.
In addition, if bar-coding of slides is deployed in the lab, then the bar-code can be scanned and decoded by the whole slide scanner and used by the DPS to automatically associate the scanned image with the glass slide,previously accessioned in the LIS in the case context.
The bar-code is a unique ID for the digital image, to ensure a valid electronic chain of custody. Finally, when the pathologist views the images and adds annotations and results of quantitative analyses to them, then these are also stored in association with the digital images (in a case context, in some DPS’s).
The DPS needs to ensure that this data remains associated with the images and can be retrieved easily for use in the clinical workflow.

Photo credit: http://www.virtualpathology.leeds.ac.uk/public/viewer/
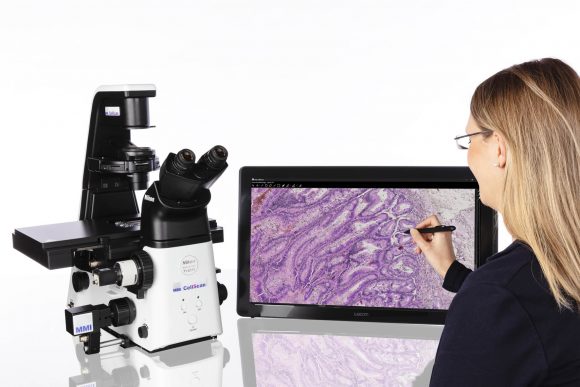
Photo credit: https://www.molecular-machines.com/blog/new-whole-slide-imaging-system-from-mmi-the-experts-in-microscope-based-microdissection
REGULATORY MILESTONES OF WSI IN USA
- 2000 - Introduction of commercial WSI devices results in Interest in digital pathology peaked. Validation of diagnostic applications
- 2009 - FDA (Food and Drug Administration) advisory panel assembled results in WSI scanners designated high‑risk Class III devices. Nonclinical use cases expand. Digital Pathology Administration and FDA discussions ensue.
- 2015 - Technical Performance Assessment guidelines released results in Assures manufacturers follow the same standards
- 2017 - FDA approval of WSI results in Approval for primary diagnosis of surgical pathology only
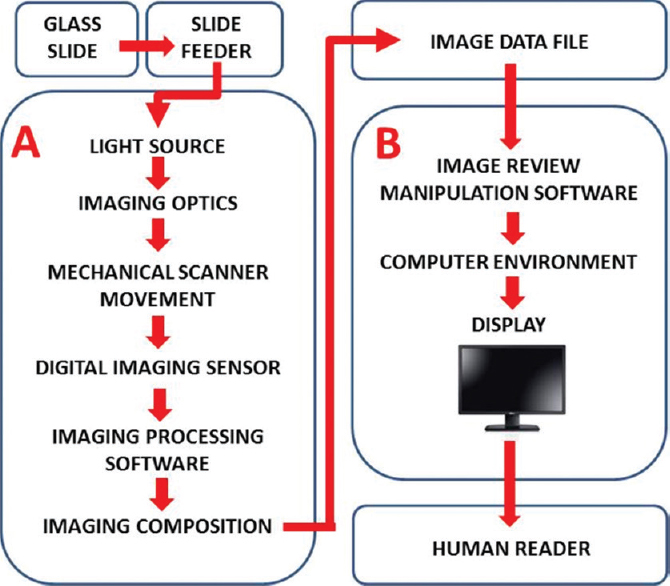
Overview of a digital pathology system. A digital pathology system is composed of two subsystems: (A) Image acquisition and (B) workstation environment. The arrows depict the pixel data pathway.
Photo credit: http://www.jpathinformatics.org/viewimage.asp?img=JPatholInform_2017_8_1_23_206226_f1.jpg
ARTIFICIAL INTELLIGENCE IN DIGITAL PATHOLOGY
AI in digital pathology also has the ability to radically change the patient experience – with apps and mobile devices giving them direct access to everything from their electronic health records (EHR) to their radiology images.
However, AI in digital pathology is enabling an even greater and profound impact on the patient experience.
New capabilities enabled by AI and emerging technologies is allowing patients to be much more engaged with their treatment
From the moment the patient comes in for a diagnostic test, the goal should be to remove as much subjectivity from the process as possible.
AI offers the ability to present computational guidance and analysis and contextualize their digital pathology data with references to genomics and other population-based health data.
Google recently developed an AI algorithm called LYmph Node Assistant (LYNA) that’s drawing attention from people who work in digital pathology.
- Advantages of AI includes
- More Personalized Treatments
- Improved Efficiency
- Positive Changes to Workflows
- More Accessible Technology
- More Time Devoted to Cases

Evolution of AI in digital pathology
Photo credit: https://www.nature.com/articles/s41571-019-0252-y
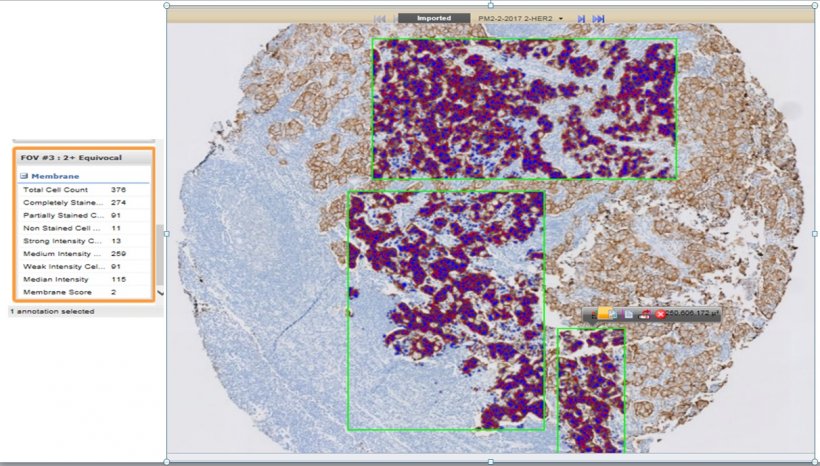
A screenshot of quantitative image analysis (QIA) of a breast cancer biomarker human epidermal growth factor receptor 2 (HER2) immunohistochemical (IHC) testing by a FDA-approved commercial platform.
Photo credit: https://healthcare-in-europe.com/en/news/unleashing-the-power-of-digital-pathology-for-precision-medicine.html
IMPACT OF DIGITAL PATHOLOGY
Benefits patients by means of permitting the fast referral of cases between organisations or across pathology networks, enhancing access to professional recommendation and opinion on diagnoses
Improves laboratory workflow and connectivity and will increase flexibility and efficiency of the workforce, assisting create digital training resources that help the development of specialists in training
Increases our power to proportion slides and more, making it simpler for others to advantage from the great information in our profession
Sets the scene for the use of artificial intelligence to be able to assist carry advances to pathology services
ADVANTAGES AND LIMITATIONS OF DIGITAL PATHOLOGY
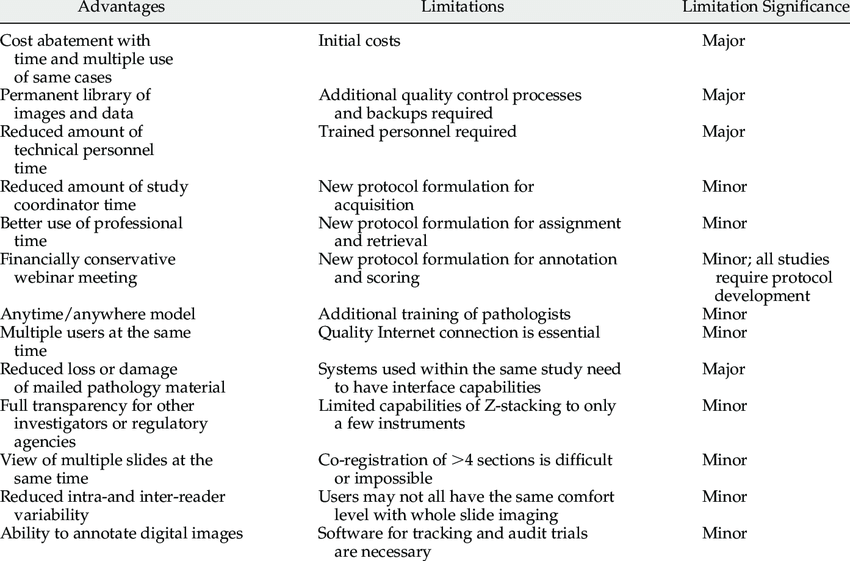
Photo credit: Digital Pathology Evaluation in the Multicenter Nephrotic Syndrome Study Network (NEPTUNE) - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Advantages-and-limitations-of-digital-pathology_tbl1_23542304
[accessed 31 May, 2020]
TELEPATHOLOGY
Telepathology is that the follow of pathology at a distance. It uses telecommunications technology to facilitate the transfer of image-rich pathology knowledge between distant locations for the needs of diagnosis, education, and research.
Performance of telepathology needs that a specialist selects the video pictures for analysis and therefore the rendering of diagnoses.
The employment of "television microscopy", the forerunner of telepathology, didn't need that a specialist have physical or virtual "hands-on" involvement within the choice of microscopic fields-of-view for analysis and diagnosis.
An academic pathologist, Ronald S. Weinstein, M.D., coined the term "telepathology" in 1986.
In a medical journal editorial, Weinstein made public the actions that might be required to make remote pathology diagnostic services.
He and his collaborators revealed the primary scientific paper on robotic telepathology.
Weinstein was also granted the primary U.S. patents for robotic telepathology systems and telepathology diagnostic networks.
Weinstein is understood to several because the "father of telepathology".
In Norway, Eide and Nordrum enforced the primary property clinical telepathology service in 1989;this remains operative decades later.
A number of clinical telepathology services have benefited several thousands of patients in North America, Europe, and Asia.
Telepathology has been with success used for several applications, as well as the rendering of histopathology tissue diagnoses at a distance.
Indeed, a number of research groups have developed and demonstrated a rich set of methods including deep learning for carrying out quantitative microscopy analyses.
However, to bring this vision to reality, it will be necessary to develop and deploy infrastructure to scan, catalog, and store extremely large collections of WSI, both for clinical work and research.
In conclusion, although the concept of the virtual microscope is two decades old, the adoption of digital pathology informatics tools in clinical practice is clearly still a work in progress.
REFERENCE
- Pantanowitz L, Sharma A, Carter AB, Kurc T, Sussman A, Saltz J. Twenty years of digital pathology: An overview of the road travelled, what is on the horizon, and the emergence of vendor-neutral archives. J Pathol Inform 2018;9:40
- https://hitconsultant.net/2019/11/22/5-ways-artificial-intelligence-is-transforming-digital-pathology/#.XtOgdrdX5kw
- Elizabeth Chlipala, Jesus Elin, Ole Eichhorn, Malini Krishnamurti , Richard E. Long, Bikash Sabata, Matthew Smith.Archival and Retrieval in Digital Pathology http://www.digitalpathologyassociation.org/
- https://www.microscope.com/education-center/microscopes-101/history-of-microscopes
- Anil V. Parwani. Next generation diagnostic pathology: use of digital pathology and artificial intelligence tools to augment a pathological diagnosis https://doi.org/10.1186/s13000-019-0921-2
- https://en.m.wikipedia.org/wiki/Virtual_microscopy
- https://en.m.wikipedia.org/wiki/Telepathology








0 Comments